ACL rehab is a challenging journey, and dealing with patellar or quadriceps tendon graft site pain can make it even tougher. In this blog post, we’ll explore the factors that can contribute to patellar and quadriceps tendon graft site pain and how to manage it effectively.
A patellar tendon autograft is harvested via a vertical strip of the patellar tendon (below the kneecap) often along with a piece of the bone from the bottom of the patella (kneecap) and tibia (shinbone) on either end.
A quadriceps tendon autograft is harvested via a vertical strip of the quadriceps tendon (just above the kneecap) sometimes along with a piece of the bone from the top of the patella (kneecap) on one end.
Both graft options are harvested from key structures that make up the knee extensor mechanism, pictured below.
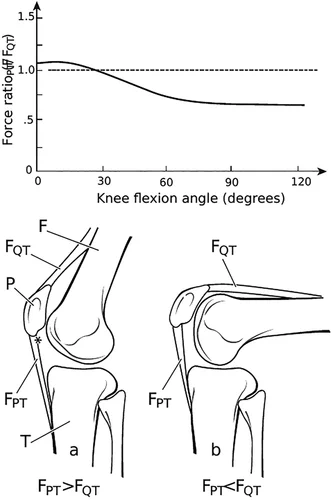
Figure 2 from Dan et al
Tendon Anatomy & Physiology
Tendons are strong, elastic structures that connect muscles to bones. Their main function is to transmit the force generated by muscles to bones, thus allowing for movement to occur.
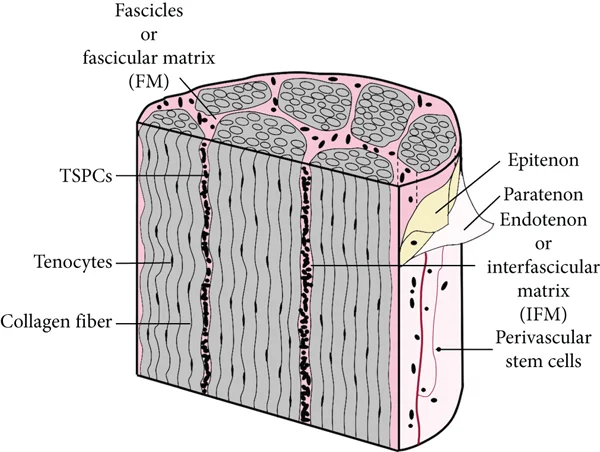
Tendons are composed of bundles of collagen fibers called fascicles, and a water-based gelatinous structure called the interfascicular matrix.
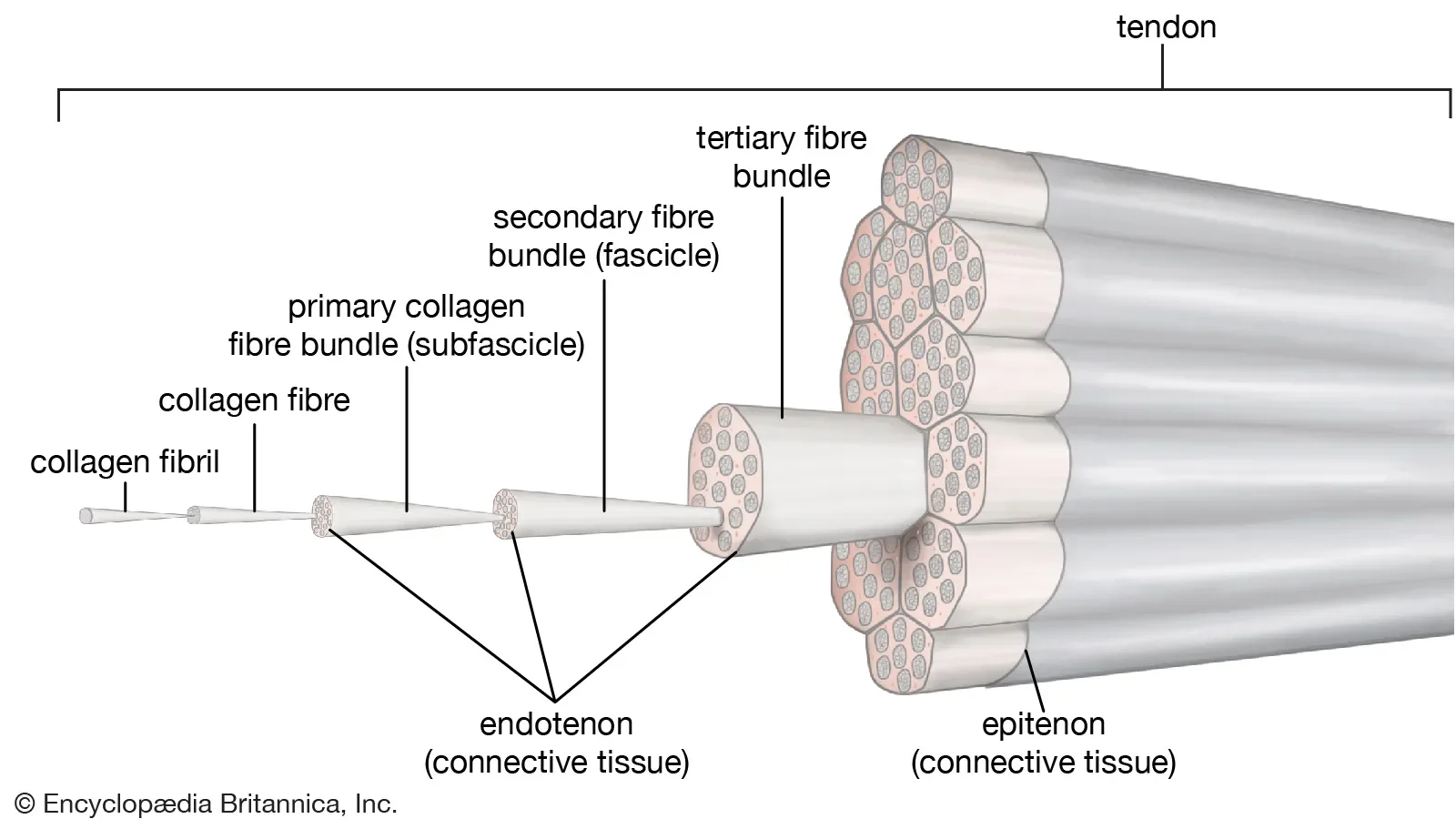
Collagen fibers are oriented lengthwise into fascicles, much like the cables in a suspension bridge. This provides tendons with their immense tensile strength, stiffness, and extensibility.
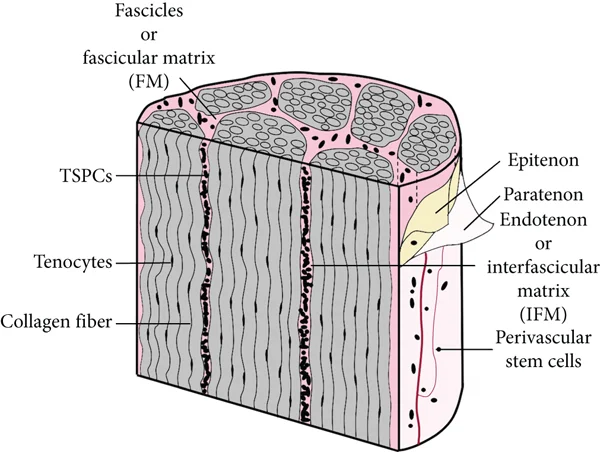
Figure 1 from Zhang et al
The interfascicular matrix (IFM) is a water-based gel structure interspersed between fascicles. The IFM provides tendons with their elasticity and allows fascicles to slide next to each other. The IFM also disperses multidirectional forces which helps to protect the fascicles.
“TENDONS ARE DUMB.”
Tendons have limited blood flow and slow metabolic turnover within fascicles, which allows them to handle immense amounts of force on a regular basis with limited tissue damage. Therefore tendons are very resilient but slow to recover if injured.
While it seems logical to blame persistent anterior graft site pain solely on the slow metabolic and healing capabilities of the donor tendon… the current body of evidence suggests this would be a gross oversimplification of tendon-related pain, even in the context of patellar and quadriceps autografts.
Tendinopathy
According to Scott et al, tendinopathy is defined as persistent pain and loss of function pertaining to the mechanical loading of a tendon. Tendinopathy is sensitive to both the intensity and speed of loading. Approaching persistent patellar tendon and quadriceps tendon graft site pain through the lens of tendinopathy can empower athletes with the tools to keep progressing throughout the ACL rehab process.
Models of tendinopathy classification and research shed light on the complex relationship between pain, structure, and function:
- Tendon pain can impair function, leading to decreased load tolerance, muscle strength, and motor control.
- Structural changes commonly occur in tendons with or without pain.
- Pain can improve without structural changes.
- Function can improve without changes in structural pathology, with or without changes in pain.
This complexity highlights the need for a comprehensive approach to managing graft site tendinopathy during ACL rehab.
Management
The goals for graft site tendinopathies are:
- Improve tolerance to loading.
- Improve function.
Eliminating tendon pain entirely is not a primary objective. Instead, the focus shifts to understanding and defining what level of pain is tolerable for the individual athlete. Consistently engaging in regular resistance training and conditioning is a crucial component of both ACL rehab and graft tendinopathy management. This is why complete rest is not recommended.
Symptom Feedback Loops
The Traffic Light Guide is a valuable framework for monitoring pain during exercise. It is designed to help you gauge what is tolerable.
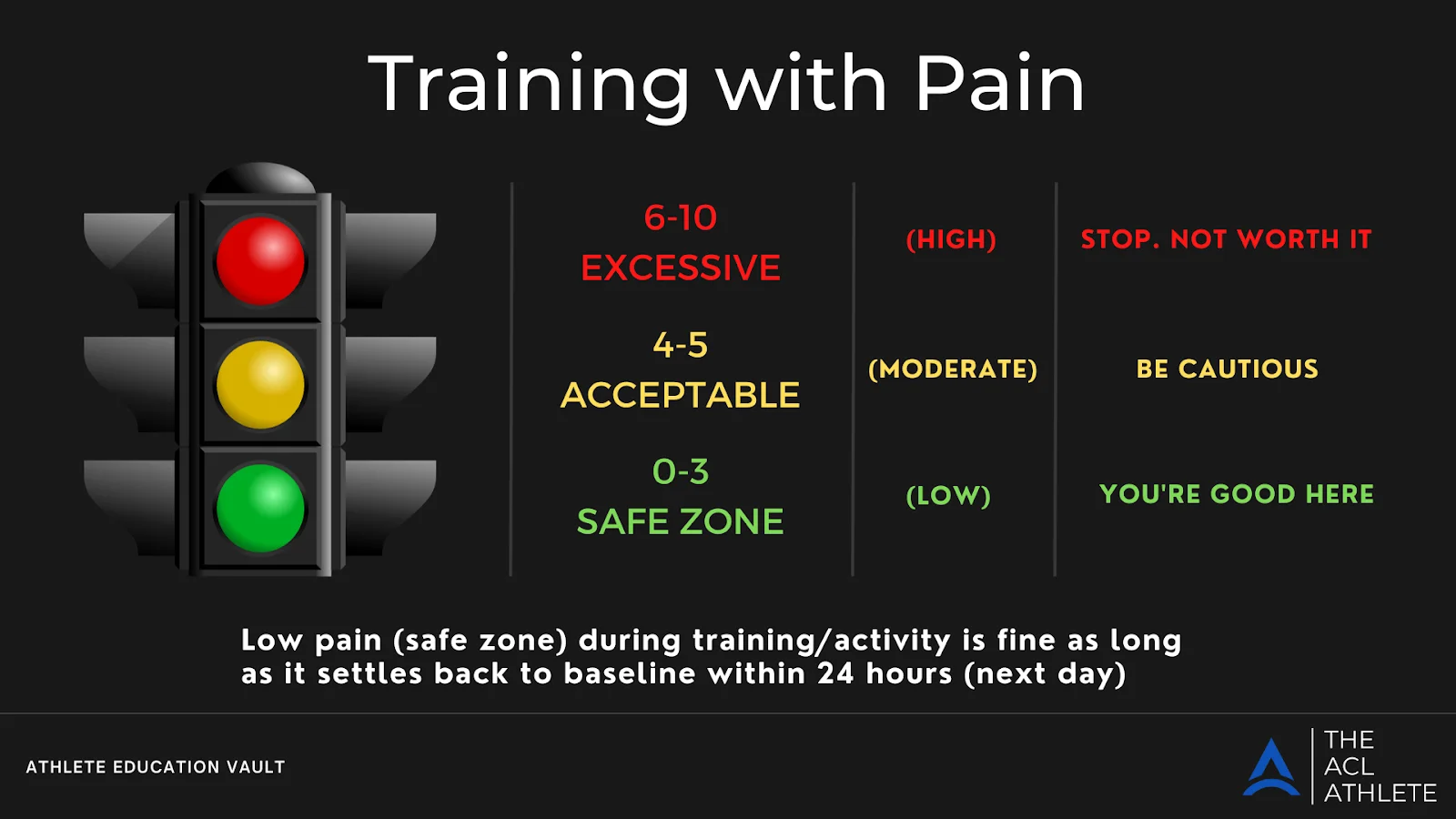
The goal with using the Traffic Light Guide is to keep symptoms in acceptable zones during exercise.
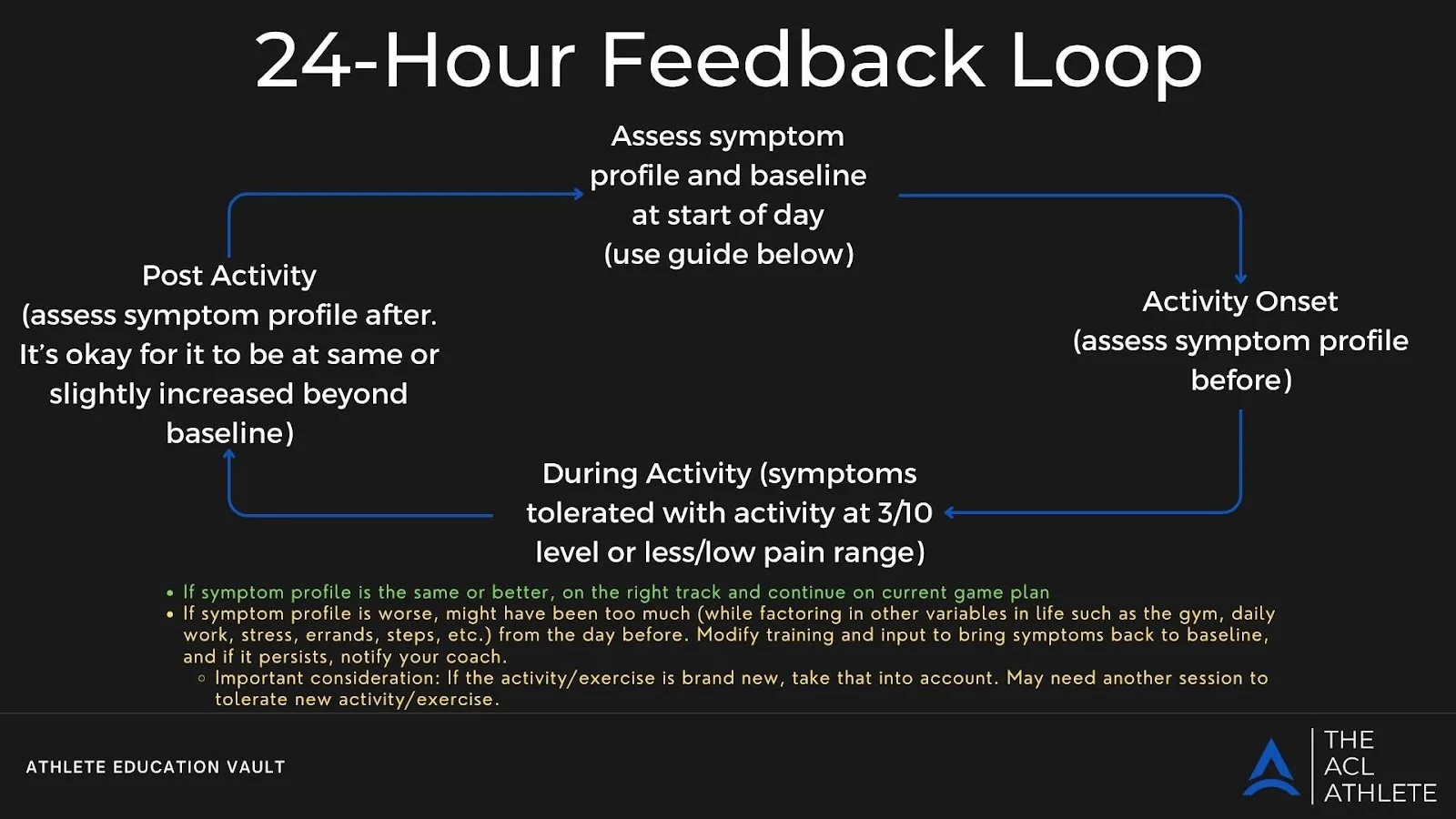
Monitoring how your symptoms respond in the 24 hours after activity can provide helpful insight to make sure that exercise intensity, volume, and frequency are appropriate for your current status. If symptoms increase the next day, it doesn’t necessarily indicate harm but suggests the need to reduce or adjust exercise intensity, volume, or frequency.
Assessing Function & Load Tolerance
Assessing function involves periodically using knee extensor-dependent movements, exercises, or activities that provide quantifiable results and allow for benchmarking based on your goals. For example, a single leg step up/step down for maximal reps, walking distance with your dog, and your 5k run time can all serve as a measure of function.
Commonly used measures in ACL rehabilitation like peak quadriceps torque, peak quadriceps torque to body weight ratio, limb symmetry index, and rate of force development are valuable indicators of load tolerance. If objective measures like these are not available, rep maxes for exercises like knee extensions, step ups, leg press, squats, and various jumps can help gauge load tolerance over time.
How do we improve load tolerance and function?
To improve load tolerance and function, you have to gradually and progressively load the tendon. Isometrics and heavy, slow resistance training are recommended methods to improve tolerance to magnitude of load.
A general recommendation to use isometrics is to gradually progress to 3-5 sets of 45-60 seconds at an intensity of RPE 7-8/10. This can be performed up to multiple times daily, 3-4 times per week, or prior to your training as part of a warm up.

A heel elevated wall sit is a great option for isometric loading. Less knee bend biases load to the patellar tendon, while deeper knee bend biases the quadriceps tendon. External resistance can be easily added to reach adequate intensity.
A general recommendation to employ heavy, slow resistance training to improve load tolerance is to gradually progress to 3-4 sets of 6-12 repetitions with a 3-4 second eccentric tempo at an intensity of RPE 7-9/10 with a frequency of 2-3 times per week.

Squat variations like this tempo box squat can be utilized to encourage adequate loading. In this instance the shortened depth and forward knee/upright trunk positioning is biased for patellar tendon loading.
To improve tendon tolerance to rate of loading, athletes can incorporate plyometric and jumping exercises. Progressing from lower-intensity plyometrics to higher-intensity tasks allows for gradual exposure to higher rates of loading and tendon stiffness. Recommendations for intensity, volume, and frequency of plyometrics will vary depending on your situation. Consult with your rehab clinician or coach for guidance.

Hops, jumps, and skips can be easily scaled and dosed based on your specific needs.
In conclusion, managing patellar and quadriceps tendon graft site pain in ACL recovery is an endeavor that takes time, patience, and consistency. By focusing on improving load tolerance and function rather than entirely eliminating pain, you can continue to make progress in your ACL journey.
References:
Marques FDS, Barbosa PHB, Alves PR, Zelada S, Nunes RPDS, de Souza MR, Pedro MDAC, Nunes JF, Alves WM Jr, de Campos GC. Anterior Knee Pain After Anterior Cruciate Ligament Reconstruction. Orthop J Sports Med. 2020 Oct 27;8(10):2325967120961082. doi: 10.1177/2325967120961082. PMID: 33195725; PMCID: PMC7605008.
Hardy A, Casabianca L, Andrieu K, Baverel L, Noailles T; Junior French Arthroscopy Society. Complications following harvesting of patellar tendon or hamstring tendon grafts for anterior cruciate ligament reconstruction: Systematic review of literature. Orthop Traumatol Surg Res. 2017;103(8S):S245-S248. doi:10.1016/j.otsr.2017.09.002
Dan, M., Parr, W., Broe, D., Cross, M. and Walsh, W.R. (2018), Biomechanics of the knee extensor mechanism and its relationship to patella tendinopathy: A review. J. Orthop. Res., 36: 3105-3112. https://doi.org/10.1002/jor.24120
Chuanxin Zhang, Jun Zhu, Yiqin Zhou, Bhavani P. Thampatty, James H-C. Wang, “Tendon Stem/Progenitor Cells and Their Interactions with Extracellular Matrix and Mechanical Loading”, Stem Cells International, vol. 2019, Article ID 3674647, 10 pages, 2019. https://doi.org/10.1155/2019/3674647
Scott A, Squier K, Alfredson H, et al. ICON 2019: International Scientific Tendinopathy Symposium Consensus: Clinical Terminology. Br J Sports Med. 2020;54(5):260-262. doi:10.1136/bjsports-2019-100885
Cook JL, Rio E, Purdam CR, Docking SI. Revisiting the continuum model of tendon pathology: what is its merit in clinical practice and research?. Br J Sports Med. 2016;50(19):1187-1191. doi:10.1136/bjsports-2015-095422
Docking SI, Rio E, Girdwood MA, Hannington MC, Cook JL, Culvenor AG. Physical Activity and Investigation With Magnetic Resonance Imaging Partly Explain Variability in the Prevalence of Patellar Tendon Abnormalities: A Systematic Review With Meta-analysis of Imaging Studies in Asymptomatic Individuals. J Orthop Sports Phys Ther. 2021;51(5):216-231. doi:10.2519/jospt.2021.10054
van Ark M, Rio E, Cook J, et al. Clinical Improvements Are Not Explained by Changes in Tendon Structure on Ultrasound Tissue Characterization After an Exercise Program for Patellar Tendinopathy. Am J Phys Med Rehabil. 2018;97(10):708-714. doi:10.1097/PHM.0000000000000951
Langberg, H., Skovgaard, D., Petersen, L.J., Bülow, J. and Kjær, M. (1999), Type I collagen synthesis and degradation in peritendinous tissue after exercise determined by microdialysis in humans. The Journal of Physiology, 521: 299-306. https://doi.org/10.1111/j.1469-7793.1999.00299.x
Cardoso TB, Pizzari T, Kinsella R, Hope D, Cook JL. Current trends in tendinopathy management. Best Pract Res Clin Rheumatol. 2019;33(1):122-140. doi:10.1016/j.berh.2019.02.001
Malliaras P, Cook J, Purdam C, Rio E. Patellar Tendinopathy: Clinical Diagnosis, Load Management, and Advice for Challenging Case Presentations. J Orthop Sports Phys Ther. 2015;45(11):887-898. doi:10.2519/jospt.2015.5987
Kongsgaard M, Qvortrup K, Larsen J, et al. Fibril morphology and tendon mechanical properties in patellar tendinopathy: effects of heavy slow resistance training. Am J Sports Med. 2010;38(4):749-756. doi:10.1177/0363546509350915
Baar, K. (2019). Stress Relaxation and Targeted Nutrition to Treat Patellar Tendinopathy. International Journal of Sport Nutrition and Exercise Metabolism, 29(4), 453-457. https://doi.org/10.1123/ijsnem.2018-0231