Show Notes:
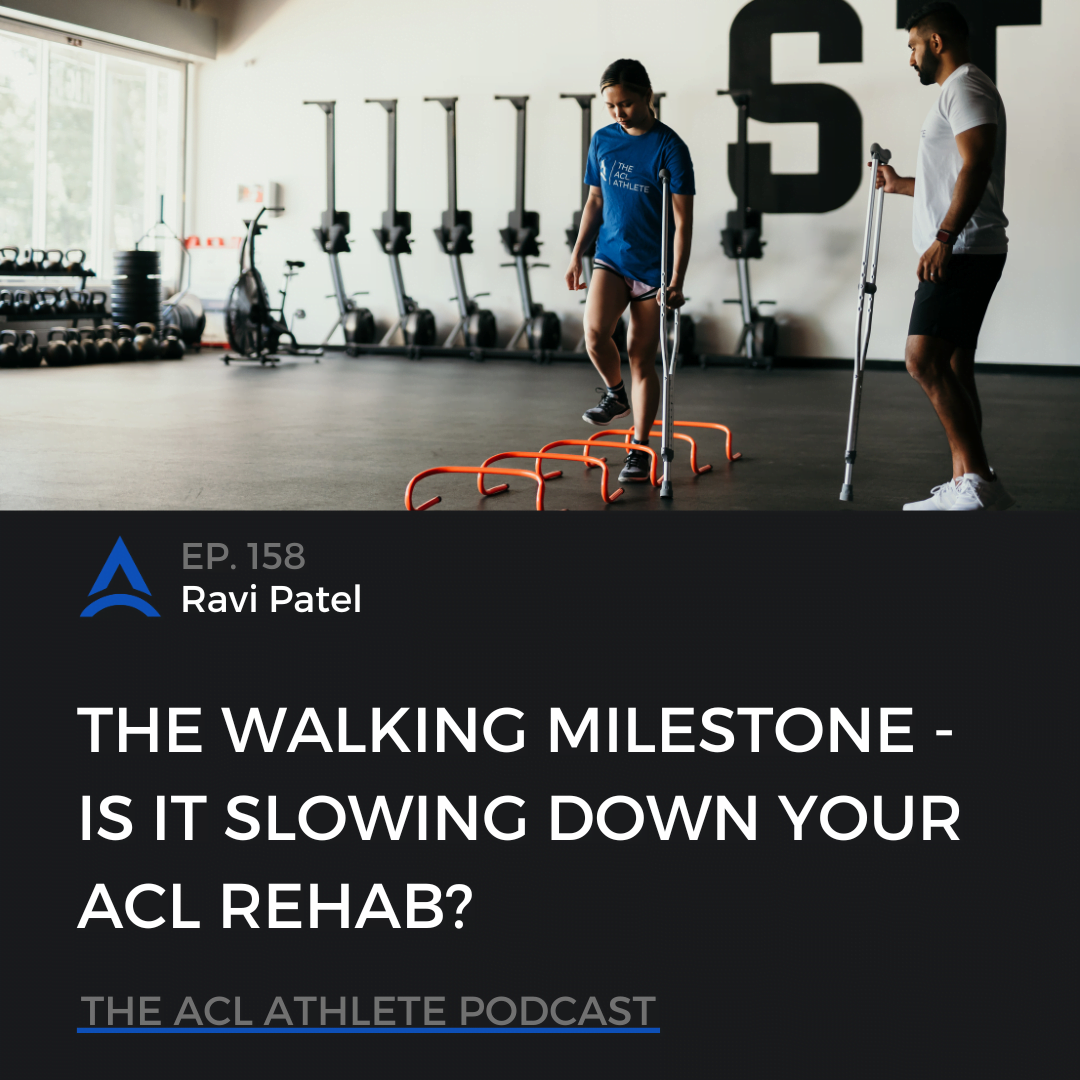
In this episode, we discuss why the walking milestone could be slowing down your ACL rehab. We talk about how this usually happens, what we see with athletes coming in, common problems and concerns, practical application of tracking and exposing yourself appropriately, and making sure your priorities are also dialed in to make sure you make the most of each phase you’re in.
What is up guys, and welcome back to another episode on the ACL Athlete Podcast. Today, we are diving into this topic: The Walking Milestone – Is It Slowing Down Your ACL Rehab? And this is something that can apply to both operative or people with an ACL reconstruction or an ACL repair. And it also applies to our non-operative ACL, but especially for our post-op, because this is what we tend to see most with our athletes that I’m going to talk about today.
This is something that is a big milestone, the walking milestone for our ACLers, especially early post-op. People are itching to get off of their crutches and get rid of those things. And so people will stop wondering what’s wrong with that person and looking weird at you or staring, always hated that. This is something that a lot of people just want to get rid of, get back to their normalcy, their independence. It takes a lot less energy and a lot less time to get somewhere.
That was the other thing too, is that, especially when you’re early postop, you’re kind of lugging around this brace, if you have a brace. And you’re just kind of swinging this leg around. Therefore, as soon as you could start putting weight on it, as soon as you can start to get rid of one of their crutches and then eventually get rid of both crutches, then that’s the freedom that we’re starting to feel. And achieving that walking milestone is a very, very big deal.
But today, I want to talk about how this milestone can actually get you into trouble and it can potentially slow things down in your ACL rehab. The thing that happens is that most people just get a green light to start walking without their crutches. You either go to the surgeon or you go to your physical therapist or you maybe decide on your own. I know many of you probably listening, you’ve been told to use one crutch, or you’re like, it’s fine. I could put weight on it. And then you slowly start to get confident and then you start just hobbling around. Even if you have been told to keep your crutches with you. I know some of my athletes have definitely done this and they come in and they’re like, yeah, I’ve been trying to like get to the bathroom without my crutches. I know you guys are shaking your head – yes.
But you get this green light and you start walking without the crutches. But you’re not really given any parameters or guidance around it. You’re just like, all right, you’re good. No more crutches needed. You may ease into it a little bit just naturally, because now you don’t have crutches and you’re still kind of testing the waters here. But then after a few days and a week, and even two weeks, you’re probably cruising along, you’re fine, especially if your range of motion is coming along, your quads, all the things on the early post-op that we will be looking for. Those are the things that will help you to build up some confidence. Especially once the crutches are gone. And this is where I would proceed with caution. Hear me out here. If you are someone who has a job with a lot of steps, you’re probably ramping up pretty quickly. Nurses, teachers, people who have to walk around school a lot, going to college. There’s a lot of steps that you have to take to get to classes and just navigate the whole day. Not to mention just so your daily functional things like going to the bathroom and then just navigating your day, our daily activities of living. Those are things that can sneak in with our steps. But this is normal, right? We’re trying to get back to those things. We were doing those things before crutches, maybe it was modified.
The other thing that I’ll mention is someone who is looking to walk for exercise. You’re someone who’s a daily stroller and loves to get walks in, especially if you’re that person who used to do maybe 10,000 steps, 20,000 steps per day. I know that there is a category of people in here who just either naturally does that from their jobs and daily activities. Or maybe it’s just something that you love to do as a form of exercise in addition to other things. You just want to get that step count to 10,000, 15,000, whatever that looks like. And that’s great.
Why am I telling you to proceed with caution or why this can potentially slow you down? The thing that can happen is that whenever we get freedom to start walking, we can potentially take advantage of it. We are able to do it. We get the green light. We don’t have these parameters as I had mentioned. What can happen is that we’re starting to get more and more load and compression through the knee joint. Nothing that’s necessarily detrimental. It’s just all about how’s the knee tolerating this load and input to the system. This is where pain and swelling can really sneak in, especially swelling. This is the quad’s worst enemy and actually plays against you – continuing to develop the strength that’s needed. And of course, some things like range of motion as well. Something called arthrogenic muscle inhibition. Swelling is related to that, which can play against the quads, really trying to turn on and activate.
This is something that we want to keep at bay, especially swelling and pain because that could play against us. Because these are things that we are also trying to focus on very importantly, in those early post-op phases with range of motion and strength. Just like with anything, we need a dimmer switch approach to building this backup.
I use this dimmer switch so much in the ACL rehab process because it’s not just this on-and-off switch. You don’t just magically start walking and then you go walk 15,000 steps in a day. It’s a dimmer switch approach because you have to make sure that you manage the load on your knee and on your body and build up that tolerance and your capacity to do that. This is what I mean by making sure that we don’t have any spikes in our volume. If you think about that gradual incline, you just won’t want that spike. Let’s say you were doing maybe 2,000 steps per day and then all of a sudden you go to 10,000 steps in a day, and then you come back down. That spike in your volume will likely shock your system a little bit. Even if you think about like, let’s say you go and travel somewhere and you naturally only do 5,000 steps in a day, and then you go to this random city and walk around all of it and you’ve conquered 20,000 steps. You wake up the next day and you’re like, man, my shins are sore, my hips are sore, my foot is beat up, my heels are sore. It’s because your body’s just not used to it. And that’s the thing that can happen even for someone who has a generally healthy body. We know these things can happen and feel that.
It’s no different in the same situation with an ACLer with a knee that is healing. We want to make sure that we take this dimmer switch approach and minimize any spikes in your volume with steps. And this applies to anything. Our gym training, our on-field stuff, any of that stuff, but especially with step count early on. And I’ve seen this way too many times, whether it’s an athlete I’ve worked with, who didn’t listen to the guidance and felt fine, and then they just go off and they’re like, all right, I’m just going to go on a walk. And they felt good. They kept going. And then they feel it the next day or later on in the day, or it’s someone coming to us later. They’re two months out, three months out, even six months out. And their knee is not tolerating things still. Well, I’m still dealing with swelling and pain. This could be due to a number of factors. There are definitely a subset of people who come in and they’ve been walking a lot and their knee stays puffy. It’s something that we haven’t been able to calm down since the beginning of the surgery. And it’s because they just went greenlight and started walking a lot.
This is where we have to be cautious because it can sneak in there without us knowing. Sometimes we’ll blame other factors on this, whether it’s like a certain exercise or a certain gym session, or maybe it is something where you are blaming something you ate. There are a number of things that you can blame on this. And sure this all kind of comes back to a total, what we call allostatic load or volume and training. When we think about stress to your system it’s stress your system. But we got to make sure we put weight where it matters and where it’s going to be most important in our priorities. If you go him walking early, then that’s going to take away from certain stress that you can put in other buckets that you need, like your range of motion or your strength or your power development, things that we need to be working on.
There’s something about once an athlete starts putting weight down, their knees sometimes don’t like it. The ACL side, they’re just like, oh, what’s going on here, is starting to go through some compressive forces, some sheer forces. All the things that go on with a normal walking stride, nothing that is negative or bad in a way, but it’s just something that’s new to the knee joint, especially after an ACL injury, after an ACL reconstructive surgery. Depending on the complexity of your injury and how long those timings are, all those things play a role. And not to mention if there’s a donor side and a graft that has been taken. Your knees just going through a lot. This is something that can shock the knee a little bit—not necessarily just walking itself but when we spike it up too quickly. The same thing can happen with running. Sometimes just act up out of nowhere, just because of the nature of the compression and the cyclical loading of running. Not to mention gravity, which isn’t helping us in our lower extremities. So these are just things to factor in, and it’s not to say that you can’t walk. You’re going to walk. It’s just a matter of managing what that looks like versus just going for greenlight and allowing yourself to do that and go back to the way it was before, especially if that was a very high volume that you were doing.
It’s even more important to keep this in mind with someone who is non-weightbearing for, let’s say two weeks, four weeks, six weeks, that knee has been unloaded and has not had compressive forces through it. Maybe because it’s a complex surgery, or maybe it’s something where you had a meniscus repair. And then maybe it’s something where you can’t put weight on it for four weeks. It’s been unloaded for four weeks and it’s crazy how much our body adapts to things like that. And it can atrophy and it can do all the things we know shrivels up like a hotdog that we can see, that we’ve worked so hard for on our quads. But this is something where we want to make sure that if we are non-weightbearing for a bit, that joint could be ultra-sensitive to those compressive forces. Therefore, we need to be very mindful about gradually adding back the weight and the steps and being very progressive, like that dimmer switch that I mentioned.
And that’s why I’m saying we can’t just treat this as a free-for-all all greenlight to do as much walking as we want. A way to think about this is just like training for a marathon. You wouldn’t just go out and run 18 miles randomly. You would have a plan and progressively build that up. Maybe it’s half a mile, a mile, two miles. It depends on what your baseline is, which is another kind of principle from this. How much is your baseline within the current week or two? And then from there you would just kind of progressively build up. Often we use the 10% role so there’s no massive spike in the volume or your body doesn’t freak out when you do increase what you are doing. Because we do want to increase that, but we want to get that to a point where it’s dancing really well along with the other factors that we’re trying to build up, especially with our conditioning, our strength, our rehab stuff that we are doing. We want to make sure that all blends really well together. We want to respect this process while still doing all of our daily life things as well.
Now let’s be practical here. You guys know that it’s important to me that you walk away from this, knowing how to put this in play for yourself. Let’s do that. The goal is to ramp up slowly. My recommendation is to actually track your steps, your Apple Watch, Fitbit, and even your iPhone. These serve as great proxies for your daily step count and activity. Keep that on you and then track what your daily step count is, even if you are pre-surgery, if you’re prehab, unless you’re going non-operative then you’re just kind of cruising along. If you have surgery, then start to track how many steps you take in a day, even if it’s with your crutches. And then start to note when you do get off your crutches and how that step count changes. Then we’ve got some data to start helping us with managing how many steps we’re taking. And we’re consistently checking in on this. We’re going to start building week to week. This is something that is more important for your life, whether it is work or school. Maybe it’s just something being a parent and you’re having to take a lot of steps chasing down your two-year-old. This is something that’s important to factor in.
And while this might seem very granular, we got to get granular here because a lot of times we’re like, all right, well, manage your steps, go and do this. And then we’re like, well, how do we actually practically do this? Well, let’s figure this out by making sure we have a game plan with this. And so then therefore tracking the steps, getting that data initially of what that baseline is, and then getting an idea of what you’re trying to work towards. If you were trying to get towards a 10,000-step count and you’re only at 1000. Well, we got a little bit to go before we try to get to 10,000.
The other thing that’s going to be really key here is if you are looking to do this for exercise or just getting your step counts up. This might need to be modified initially. And we got to see how the knee responds and the tolerance to that volume of steps. With our athletes, we’ll track step counts and give recommendations based on what phase they’re in, how their knee is responding, and how important that goal is for them.
If we’re aiming for exercise or cardio four steps, then we’re going to substitute this for what we call off-foot conditioning to minimize the steps and load the joint to make sure that stress is worth what we want. Meaning that the range of motion is what we’re working on, the strength pieces. The things that are going to be really key for building up, especially the knee in the early and mid stages and not letting our walking be something that takes away from us. We want all to work synergistically to get you to a better place. But sometimes what we see is that the walking can actually be the antagonist while you’re trying to do all the things of getting the knee strong and in a better place. But it’s getting puffy or swollen and we wouldn’t recognize it unless we dug into the details. Because you might have been just accumulating steps and thinking, oh, well maybe it was that exercise I was doing. When in reality, you’re just on your feet with 10,000 to 15,000 steps, and that spiked up really high.
To give you guys a practical example. We have plenty of athletes who either come to us initially post-op or maybe they’re with us a little bit later and we have to dial this back. It’s because their knee is responding negatively to that. And we got to figure out, okay, here’s where their current baseline is, based on their testing and their assessments. And then what’s their next checkpoint we’re trying to get to? Is walking a part of that or is it something where we can maybe reduce that or modify that without impacting their life? Therefore, we can focus on some other buckets that we’re trying to fill and prioritize such as range of motion or strength, getting the quads going, getting some donor site pain down. Maybe it’s getting some position comfortable for themselves. There are a bunch of different things that we’re working on. Is walking going to be a big part of that? We don’t know. It just depends on their goal. But of course, we want to make sure that we are prioritizing the right things and it might be something where we reduce their step count.
We might work on some areas to allow better loading of the joint and then allow that to get further and further away from the surgery and the injury. And the knee is starting to normalize and respond better to the walking. We’ll build in some other ways to get conditioning in that isn’t so stressful through walking-type exercises or things where it’s very, weight-bearing heavy. We’ll do off-foot stuff like maybe it’s on a rower or a bike, battle ropes. There are a ton of different things that we can add into the mix that will allow athletes to still get that fix of cardio without feeling they need to go take a bunch of steps to feel like they’re burning calories or getting some sort of aerobic conditioning. This is where we have to come back to make sure the stress is worth what we want at this point. Of course, as once we get a bit further out, you can start adding this in more and more, as the knee responds well to it. We’re like, all right, cool. Here are our parameters. And this is where we’re going to work within.
And going back on that previous example, there are some athletes where walking isn’t necessarily a big goal for them. But let’s say that they sometimes do get above 5,000 steps and 6,000 steps and their knees for some reason or another respond negatively to it. But if they stay below that threshold, they’re good. And they can keep cruising with some of the strength stuff and feel totally great. And this is where the human body is wild. Some people have been able to progress appropriately. For some reason, they hit a certain threshold of steps and it responds negatively. I can’t explain to you why exactly. But this is something that we would just talk about as a group. I make sure that we know what the game plan is with them. And especially if that’s not a big priority, we’ll cool, let’s keep cruising. And then slowly over time, build that up and see how the knee responds and the body responds to it. This is something that I think is important for us to make sure that we touch on, because this is where it all comes back to the goal.
Unless it’s for work, school, daily life, and it’s a non-negotiable for you, we want to progress this a bit slower for walking and focus more on the other buckets of getting super strong in those quads and hamstrings and other muscle groups. Get the range of motion in a good spot. This is one as a team, we see happens a lot in sneaks and if people aren’t careful and they’ll pay the price for it, with a setback, with a swollen knee joint, or am I just feel tight and puffy and never go away. Unless we address the root cause of this or the root causes, we’re just going to kind of keep cruising along with a knee that’s operating at a 70% threshold when we could be at a better place by maybe reducing that back and putting more intent in the other areas.
This is something where we have to be smart about our overall phase goals, the direction we are going in, and how the knee is responding to it. So just be cautious. This isn’t something to say, stop walking, keep walking. And of course, it’s all going to be based on your lifestyle and goals. But let’s make sure also to dial in what that looks like alongside your other goals in your ACL rehab process and where you are.
I hope this was helpful, team. Something that can get missed a lot and can help you if you’re navigating this process and dealing with potentially some swollen knee joints. And you are someone who is walking a lot, maybe this is something to bring up with your PT or your rehab professional and see if you might need to dial it back. This is something to consider. But this is something also you can reach out to us. We’re happy to help. You can send us a message, you can send us an email, you can send us a carrier pigeon, or whatever you prefer to reach out. We love the messages. I appreciate all of you who connect with us and who ask questions and who just say, thank you. We appreciate you so much. That’s going to be it for today, guys. Until next time, this is your host, Ravi Patel, signing off.
Subscribe and leave The ACL Podcast a review – this helps us spread the word and continue to reach more ACLers, healthcare professionals, and more. The goal is to redefine ACL rehab and elevate the standard of care.
Resources:
- Check out our free ebooks on our Resources page
- Sign up for The ACL Athlete – VALUE Newsletter – an exclusive newsletter packed with value – ACL advice, go-to exercises, ACL research reviews, athlete wins, frameworks we use, mindset coaching, blog articles, podcast episodes, and pre-launch access to some exciting projects we have lined up
- 1-on-1 Remote ACL Coaching – Objective testing. An individualized game plan. Endless support and guidance. From anywhere in the world.
- More podcasts? Check out our archives
Connect: